"In Derbyshire we have utilised the iBCF to meet demand head-on and this has led to a reduction in delayed transfers of care. The next step is to look at how to manage demand differently, focusing on maximising people’s independence and resilience to reduce, prevent and delay the need for acute health and long-term adult social care.”
The two billion pound question
Is there an opportunity to move from meeting to managing demand? Reframing demand at the health and care interface.
The Context
This report is being published on the anniversary of the Government’s announcement of an additional £2 billion for adult social care in the 2017 Budget.
The last 12 months has been a rollercoaster for those working at the frontline of adult social care. Late announcements, hastily developed and subsequently delayed guidance, and the corresponding bunfight between Government Departments, NHS England and the Local Government Association (LGA) over the appropriate use of the funding, have often masked a fundamental positive: namely that the Government recognised that success at the interface between health and care could only be realised if the two systems worked in sync. However, it was never going to be easy to deliver sustainable change in such a short timeframe.
The additional £2 billion over three years gave local authorities a lifeline in a time of crisis. They breathed a huge sigh of relief and proceeded to:
- revisit transformation plans and initiatives that had been shelved as demand for traditional services continued to rise and funding became tighter;
- revisit ambitious savings plans that were a stretch to deliver; and
- engage with home care providers, offering additional resources to meet needs.
With £1 billion of the funding almost spent, and another £1 billion to be invested by March 2020, this is a timely moment to ask what has been achieved so far and to reflect on how the rest of the funding could best be used.
For more information about the Better Care Fund (BCF) and the Improved Better Care Fund (iBCF) which this money supports, see the LGA website.
Contents
How it was announced
“The government will provide an additional £2 billion to councils in England over the next 3 years to spend on adult social care services. £1 billion of this will be provided in 2017-18, ensuring councils can take immediate action to fund care packages for more people, support social care providers, and relieve pressure on the NHS locally. Building on the approach to the Better Care Fund, councils will need to work with their NHS colleagues to consider how the funding can be best spent, and to ensure that best practice is implemented more consistently across the country. This funding will be supplemented with targeted measures to help ensure that those areas facing the greatest challenges make rapid improvement, particularly in reducing delayed transfers of care between NHS and social care services. Overall, local government will be able to increase social care-specific resources in real terms in each of the remaining 3 years of the Parliament.”
HM Treasury’s Spring Budget 2017 policy paper, published 8 March 2017
About this Report
This report shares findings from the IMPOWER Collaborative. The Collaborative has brought together leading local authorities and their health partners to share best practice around investing the extra £2 billion of social care funding.
It has helped its members create value and demonstrate impact, as well as plan their investments in subsequent years.
- The Collaborative provides its members with:
- Assurance and confidence that their investments are maximising value for money
- A robust evidence base to support assessment of value for money
- Access to a growing network of councils to maximise shared learning
- A wider system view across health and social care
- The opportunity to contribute to the national debate on iBCF
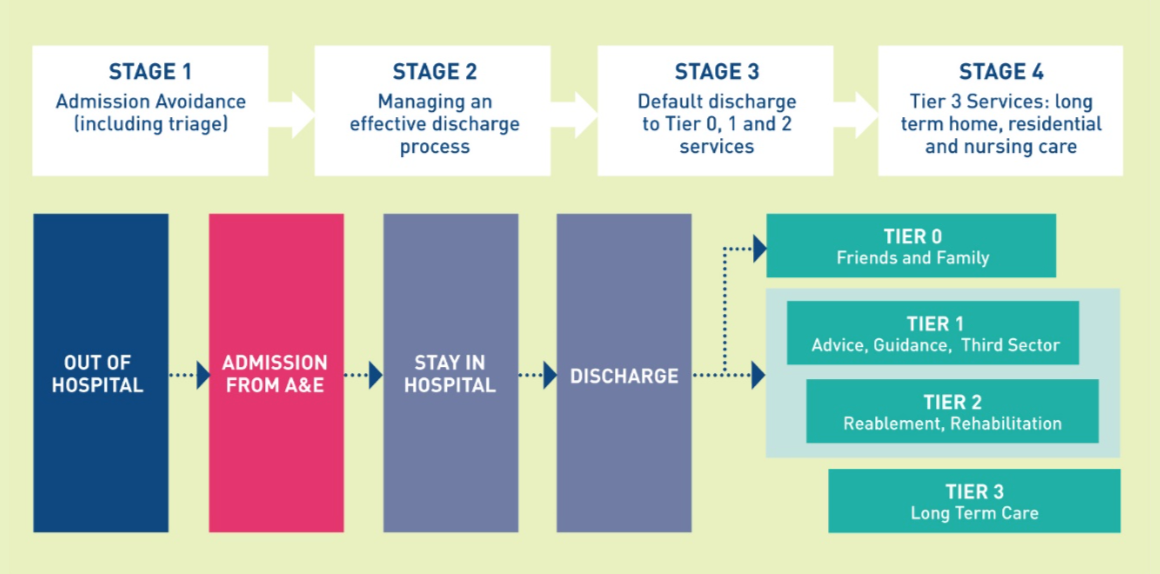
More than 15 councils were involved in the Collaborative in 2017-18, enabling IMPOWER to analyse £126 million of spending plans (approximately 12.5% of the national allocation) as well as forecast outturns. The plans were evaluated against a simplified best practice model of the care system, showing opportunities for the NHS and Adult Social Care Departments to work together (illustrated in figure 1).
Of local government spending analysed
Executive Summary
Will the extra £2 billion promote a much-needed step-change at the health and care interface, enabling both systems to work better together in the interests of users? Or will it have been just a temporary funding fix that ultimately changed very little?
IMPOWER has worked with 15 Councils over the course of the year, undertaking detailed quantitative and qualitative analysis of £126 million-worth of spending plans (one-eighth of the national allocation). In addition to face to face meetings on the challenges, our in-depth work with a selection of Councils helped to establish an evidence base behind investment decisions, canvass opinions through a survey, and test the conclusions drawn within the report at a facilitated event. We also established a Steering Group of Directors of Adult Social Care and wider industry experts in debating the findings and developing the conclusions. The report provides summary analysis and conclusions from this work – further detailed analysis is available on request. We thank the participants for their time, including those who offered comments on this report.
This report argues that, whilst the funding has helped to meet demand within the system through reduced delayed transfers of care, sustainable change is only possible if the £2 billion is used to manage demand, not just meet it.
Political pressure to spend the money quickly to see an immediate fall in delays in hospital discharge (DTOC) has almost overwhelmed other health and social care priorities. Initiatives over the last year that did address demand (for example through admission avoidance) were effectively going against the flow. While low, the fact that 8.5% of the money used so far was spent on addressing demand is a very positive indicator of how some councils could resist the pressure to simply plug funding gaps to meet demand. Ultimately however, the key success measure will be whether we can get that figure higher – not only as a proportion of iBCF spend, but as a proportion of all spend at the interface of health and care.
The report also argues that there are a range of barriers and concerns shared across health and social care including:
- There is a lack of robust quantitative and qualitative evidence on the outcomes and benefit trajectories of services. This prevents health and social care teams from challenging the value they receive from services, and services continue despite offering poor outcomes or value;
- Local authority Chief Executives and senior officials identified addressing inconsistent behaviours between health and social care systems as a top priority in a recent IMPOWER survey;
- The £2 billion in iBCF is just a tiny proportion of health and social care spend. Different methods of evaluation results in a disjointed response as it encourages a collection of initiatives rather than a co-ordinated approach across the whole system;
- Recruiting and retaining staff in critical roles across health and social care, particularly the home care sector, is impacting on delivering sustainable change;
- National policy through incentives, funding and behaviours from national bodies do not adequately encourage local health and social care partners to invest in prevention and maximising independence.
We propose five recommendations to addressing these issues and addressing demand.
1. Widen the lens beyond iBCF
Local authorities and health partners should replicate their iBCF collaboration across the entirety of their spend at the interface of health and social care to drive better performance and outcomes.
2. Invest in admissions avoidance
Local authorities and health partners should focus their energy and resources on jointly developing community services both to support admissions avoidance and to enable discharge to maximise independence and minimise reliance on acute and long-term care.
3. Invest in disruptive innovation that tackles behaviours
Local authorities and their partners should challenge current practices, share evidence of where services are not working, and promote alternatives which support better demand management. Addressing unhelpful behaviours that result in greater dependency for the user and higher costs across the interface of health and social care should be a top priority.
4. Address workforce issues jointly
Within local areas, councils and NHS partners should develop system-wide strategic workforce plans including a career framework across health and care roles to ensure that they are able to recruit and retain the right skills and maintain the capacity and capability needed to deliver care to the local population.
5. Change the narrative from coping with demand to maximising independence
Whitehall Departments should incentivise councils and healthcare providers to prioritise efforts related to improving long-term independence and resilience rather than hospital admissions or long- term care.
Delivering these recommendations requires agreement and collaboration between local councils, health partners and national health and care bodies. There is a clear opportunity over the next two years; it needs to be seized if we are to create a more sustainable system.
Analysis of Spending Plans
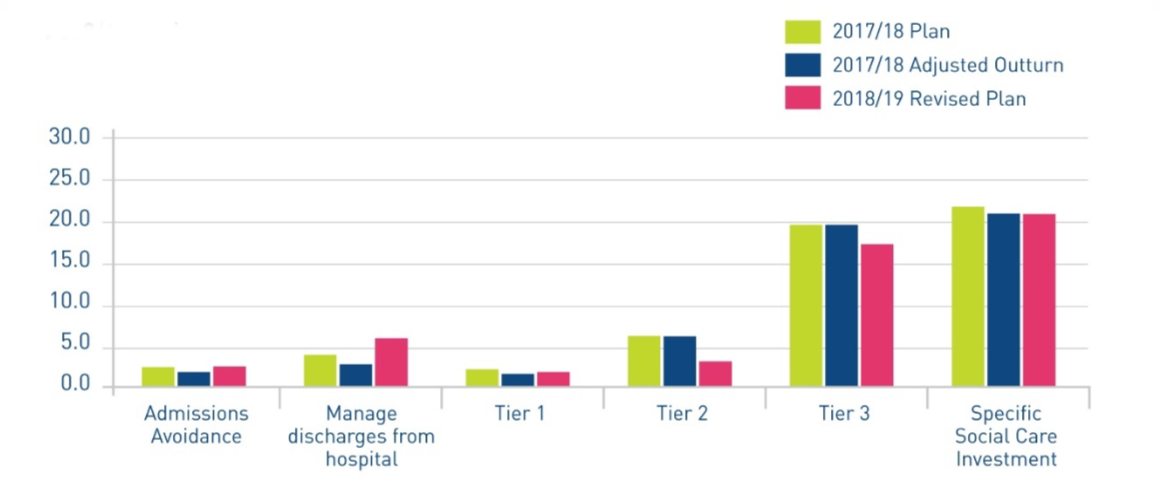
When undertaking our analysis of the £126 million-worth of iBCF spending plans, we considered whether an investment would contribute to improving performance across both health and social care, rather than sustaining or re-investing in existing services. Figure 2 shows our analysis of the 2017/18 plans, 2017/18 adjusted forecast outturns2 and 2018/19 plans by the stages of the interface model in figure 1, with other specific social care investment shown as a separate category.
Figure 2: Analysis of iBCF plans and forecast outturn 2017/18 & 2018/19 by model stages (in £ million)
What does this, and our wider analysis of spending plans tell us? Our detailed findings have been summarised in four categories.
Findings related to 2017/18 plans:
- 72% of planned spend in 2017/18 was committed to sustaining or reinvesting in existing adult care and NHS services, including funding packages of care.
- 18% of total planned spend identified within the specific Social Care investments relates to sustaining NHS services, where funding is being withdrawn by the NHS but there is recognition within councils of the need for the services to continue. This demonstrates that councils are supporting the NHS to sustain services that would otherwise have been decommissioned.
- There is clear evidence of activity focused on improving performance – our analysis identified 127 improvement initiatives with a value of £18.5m, which enabled councils to share learning, successes and challenges, and build evidence of impact.
“Our ability to understand the impact of the investments we make is critical if we are to thrive. When we work collaboratively to understand developments, initiatives and spend patterns then we have a much richer picture than would otherwise be possible. For example, in Lincolnshire we have made good progress this year in working with our health colleagues developing access to services seven days a week that have enabled people to be discharged from hospital safely at weekends. Collaboration is a key to success in our world, however we must build this as a default into all that we do.”
Glen Garrod, Executive Director of Adult Care and Community Wellbeing for Lincolnshire County Council
Findings related to 2017/18 forecast outtrun:
- Delays in central government sign-off will result in slippage on original plans by 19% of budgets. Approximately 6% will be carried forward to fund future improvement projects; however, 13% is being used to fund current care packages, increasing the overall funding towards Tier 3 care to 45% of iBCF allocations. This is driven by the national focus (from the Health and Social Care Secretary in particular) on driving down DTOC rates.
- The national focus on DTOC, grant conditions and guidance have discouraged investment in reducing demand into hospital and Tier 3 long- term care. While credit should be given to local health and care partners for identifying the need to invest in admissions avoidance in hospital and tier 3 long-term care, only 8.5% of total allocations was invested in avoiding admissions for 2017/18, which is not enough to improve outcomes.
Said increasing demand was the key risk factor in delivering against plans
Recent surveys of Local Government Chief Executives and Directors (IMPOWER, January 2018) and NHS Finance Directors (Healthcare Financial Management Association, July 2017) indicate reducing demand for hospital and long-term care is a priority. The HfMA survey revealed that 74% of Clinical Commissioning Group Finance Directors said increasing demand was the key risk factor in delivering against their 2017/18 financial plans
Findings related to 2018/19 plans:
- Councils plan to increase spend from 24% to 30% on initiatives to improve performance. This is a positive message that investment is being maintained despite the challenges outlined above. However, this is arguably still insufficient to manage demand to the extent required.
General Findings
- We identified common challenges faced by local authorities in progressing implementation of iBCF schemes and joint working with their NHS colleagues.
- Workforce capacity and capability is a significant barrier in investing in new services: There are significant challenges in attracting, recruiting and retaining staff across a range of health and social care professions. Some 60% of respondents to IMPOWER’s survey identified the local care market as a significant barrier to improving outcomes. A functioning community offer is therefore essential to improving flow and reducing demand. A core component of this is homecare; and years of funding reductions and the growth of other lower-pressured employment opportunities have left the external homecare provider market with a reduced ability to attract a capable and compassionate workforce.
- It takes time to set up new services: The delays in iBCF plans being signed off, compounded by the time it takes to establish new services and then recruit new staff has resulted in some schemes not coming to fruition during the year, despite positive relationships and joint working between health and social care organisations.
- Lack of investment in change and programme management to support delivery: The responsibility for designing a change programme and managing its implementation often resides with middle managers, who already have a significant operational workload – resulting in slippage of new schemes or replication of existing services from a fragmented system.
- Behaviour change and system leadership are the main priorities in improving DTOC and outcomes for people: 72% of IMPOWER survey respondents identified behaviour change as the biggest priority in improving health and care outcomes, with additional capacity and investment seen as the least important priority.
Process findings:
Our analysis also extended to reviewing the process and timelines involved with the allocation of additional funding:
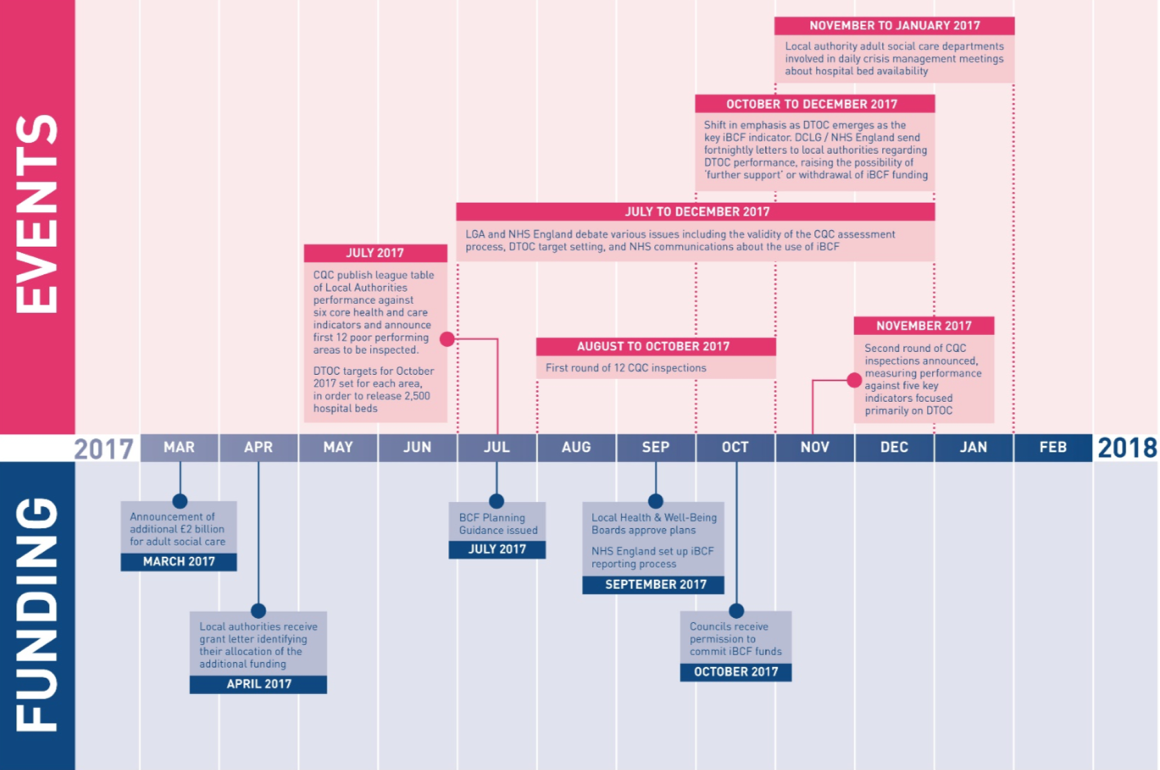
The conclusions we have drawn are significant in terms of the impact of spending:
- Winter had arrived before funding could be formally committed. Pressure to support the NHS during winter was already being applied in October. Short term fixes in the form of additional packages of care were inevitable and the risk of slippage on new services intended to improve performance was high given the delay.
- Poor regulatory and political leadership drove an even bigger wedge between the NHS and local authorities’ Departments of Adult Social Care. The behaviour of regulators4 and central government5 demonstrated poor system leadership: protectionism, personal agendas, and competing priorities dis-incentivised system working.
- Cultural gaps between local authorities and the NHS need to be addressed for systems to be successful. As local governments and officials are used to being responsive and accountable to their local populations, they do not always respond well to national pressure from political and regulatory NHS bodies.
What are the results from the £1 billion spent so far?
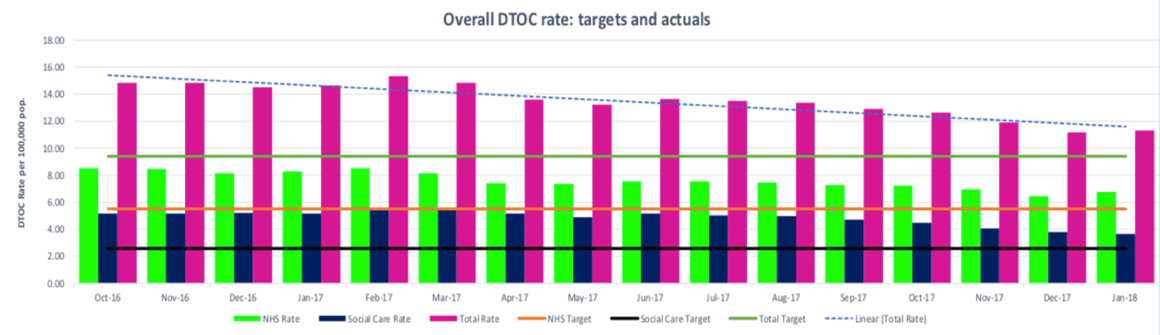
Results at the national level
Nationally, there is clear evidence that the focus on DTOC and the availability of the additional funding has had a positive impact, with an overall reduction in DTOC rates by more than 26% since February 2017. While the figures for January 2018 showed a slip backwards, it is too early to know if this was just a winter blip. Figure 4 shows the national trend.
Figure 4: DTOC rates for NHS and Social Care in England October 2016 – January 2018
Productive partnership conversations and pockets of good practice where iBCF investments have funded local integrated schemes provide evidence that the additional funding has sharpened the focus on working together at the interface with health.
However, as figure 5 shows, emergency admissions rose by 4.5% during 2017, and in January 2018 they were 7% higher than they were in January 2017.
Figure 5: Total emergency admissions September 2016 – January 2018
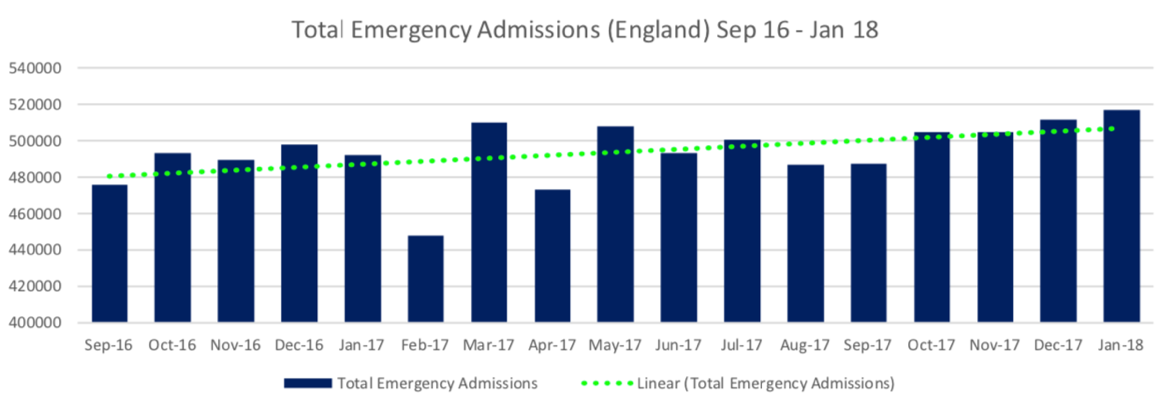
The evidence shows that although national DTOC days are falling, emergency admissions continue to rise which means that the improvement in DTOC cannot be sustainable. iBCF money provides an opportunity to manage the additional demand that rising admissions creates for services at the point of discharge in the short term. Indeed, many councils that IMPOWER is working with have indicated that demand for long-term care packages is increasing because of the focus on processing demand. However, unless iBCF funding is used to address demand at the front door (principally avoidable admissions), it will not be possible to sustain the improvement in DTOC performance and outcomes for people will deteriorate.
This poses a question – what could be achieved if there was a national focus including on incentives for admission avoidance or on developing appropriate Tier 1 and 2 services to manage discharges appropriately to prevent, reduce and delay the need for long term care?
“The report conclusions and future direction of travel resonates strongly in Somerset. Our iBCF investment in a Home First model has had a significant impact on reducing DTOC by over 40%, and our acute colleagues have acknowledged that without this the Somerset system would have fallen over and hospitals would have closed their doors. Its enabled the system to survive this winter! However, no longer is it DTOC that is the only key issue for hospital capacity, but the rise in admissions.”
Tim Baverstock, Strategic Commissioning Manager, Adult Social Care, Somerset County Council
Results for three councils: a more detailed look
IMPOWER has been working with three councils to establish evidence of impact for 19 iBCF-funded schemes across admissions avoidance, managing discharges, and Tier 1 and Tier 2 care.
Perhaps unsurprisingly, 66% of these schemes are focused on improving DTOC and reducing the length of hospital stays. Over the 19 schemes, we developed 29 different indicators which enabled the councils to establish cause and effect from individual initiatives in relation to various priorities:
Strategic level
Including system performance indicators focused on national priorities, such as DTOC and residential care volumes.
Operational level
Service level indicators focused on local priorities, enabling councils to hold services to account for delivery of outcomes.
Personal level
Person-centred outcome measures, such as the percentage of people who report that services help them control their daily lives.
Despite the challenges of implementation, there is emerging evidence that the investment is having an impact.
For example, in Derbyshire, investment in dedicated social workers in community hospitals, alongside improved joint working and communications with the community healthcare provider, is enabling frail older people to return to their place of residence more quickly, measured through a reduction in DTOC days and length of stay in community hospitals.
Graham Spencer, Group Manager – Better Care Fund, Adult Care, Derbyshire County Council
In Lincolnshire, investment in 7-day working, in conjunction with the local acute healthcare provider, has enabled weekend discharges and supported discharge planning over the past few months, leading to improvements in length of stay and reduced delayed transfers of care.
In Hertfordshire, investment in dedicated front of house teams within hospital Emergency Departments, including social workers and the voluntary sector alongside clinical navigators and existing clinical infrastructure, is speeding up discharges, reducing care packages, preventing hospital admissions and improving patient satisfaction. This is being achieved through a co-ordinated and early assessment, real-time discussions on expectations with family and carers, access to wider resources in the community; and providing support for safer early discharge from the voluntary sector.
2018/19 will be important in providing measurable evidence of impact and the councils we are working with are well placed to demonstrate these improvements.
“The introduction of the iBCF certainly saved Hertfordshire from making deep cuts to adult social care budgets in the medium term, and allowed some limited investment in bringing forward future planned inflationary increases to homecare providers to boost that fragile market. The fixed term nature of the grant has however precluded more strategic investment of this money. It has been useful to be a member of the IMPOWER Collaborative to compare how we are using the monies and adapt our plans mid-year.”
Iain MacBeath, Director of Adult Care Services, Hertfordshire County Council
Recommendations
Our analysis of iBCF spending has its limitations as such spend represents only a tiny proportion of the total spend at the interface between health and social care in England.
Nonetheless, based on the evidence obtained and conversations with both system leaders and local staff and people, we offer five key recommendations for the year ahead.
Recommendations 1-4 are for local authorities and their health partners. Recommendation 5 is for central government.
Recommendation 1: Widen the lens beyond iBCF
Local authorities and health partners should replicate their iBCF collaboration across the entirety of their spend at the interface of health and social care to drive better performance and outcomes.
The additional resources available for social care in 2017/18 through iBCF have been a core enabler for DTOC improvements and we have seen evidence of collaborative partnership working at the health and care interface.
Delivering health and care is complex, as responsibility for it is distributed across many individuals and organisations. Developing clear mechanisms for measuring the impact of iBCF investments has given local authorities a much clearer understanding of the expected benefits – even where the benefit accrues to another part of the system.
The grant conditions set out by the lead government departments – DHSC and MHCLG – included greater coordination at a local level. The IMPOWER Collaborative has shown that this has led to more joined-up decision-making, based on stronger local evidence. In the longer-term, this should drive more robust performance management both day-to-day and for future funding decisions.
The best of the 127 iBCF improvement initiatives we have seen were notable for their rapid decision- making, effective collaboration and smart evidence focus. Deploying this type of approach across all spending at the health and care interface would bring about significant improvements in performance and outcomes, as iBCF is estimated to only account for a very small proportion of total spend at the interface.
Putting in place a similar structured approach to developing an evidence base behind a greater proportion of health and social care spend at the interface, and collecting smart system-wide evidence to address local priorities, will help councils and their health partners to make constructive joint decisions around the use of increasingly scarce resources.
"We have an opportunity, through the iBCF, to support system wide change across patient and user pathways to manage demand for urgent care and reduce conversion to hospital admissions and long-term care placements. However, focus on one part of the system will only achieve a limited impact. Furthermore, this requires a whole system investment as a significant part of the activity and funding is outside of individual councils’ control.”
Carolyn Nice, Assistant Director, Adult Frailty and Long-Term Conditions, Lincolnshire County Council
Recommendation 2: Invest in admissions avoidance
Local authorities and health partners should focus their energy and resources on jointly developing community services that will both support admissions avoidance and enable discharge, to maximise independence and minimise reliance on acute and long-term care.
Of the iBCF plans reviewed through the IMPOWER Collaborative, local authorities are forecast to spend approximately 45% of their grants on sustaining and purchasing additional Tier 3 long term care packages. While this has made an impact at a national level on DTOC rates, it is clearly unsustainable in the longer term.
Managing demand is key. Within the plans that IMPOWER has reviewed, just 8.5% of iBCF grants are being invested in avoiding hospital admissions. Not only is this insufficient to transform services at the front door of A&E, but also falls short in the context that emergency admissions rose by 4.5% over the past year. In driving down DTOC rates, we have neglected to address the cohorts of people whose admission and subsequent transfer of care could have been avoided in the first place.
This is not a criticism of local authorities as the incentives in the system and guidelines on use of resources encouraged investment in specific areas; however, maintaining this approach will increase the demand on an unsustainable system.
To support this recommendation, system leaders need to work together to:
- align organisational and system incentives;
- establish joint funding mechanisms that support local system decision-making (going beyond the existing BCF arrangements); and
- develop local health and care system measures that prioritise decision-making around avoiding admissions and strengthening an intermediate care offer.
"In addressing the issues and manage demand in the system, the emphasis needs to be on developing local and regional budgets and mechanisms that incentivise the flow of money away from acute secondary care into admission avoidance, community reablement and ultimately in prevention and wellbeing.”
David Watts, Director for Adult Services, City of Wolverhampton Council
Recommendation 3: Invest in disruptive innovation that tackles behaviours
Local authorities and their partners should challenge current practice, share evidence of where services are not working and promote alternatives which support better demand management.
IMPOWER’s analysis shows that the current decision-making processes within and between local authorities and health partners continue to promote models where patients are pushed into long- term care. This narrative directly contradicts a cornerstone of all local plans – the aim of better managing demand. This objective involves maximising the independence of individuals to improve outcomes for people, as well as creating a sustainable system for public services, to move towards providing care outside of hospitals and long-term care settings.
System leaders must challenge those services and approaches that do not align with these aims, to learn from failures and to take action to address them. A priority in understanding and learning from failure is to address the need for behavioural change between local authority departments of adult social care and their health partners. In making these challenges, there must be evidence that shows why the services identified do not work and what the alternatives would be.
Recommendation 4: Address workforce issues jointly
Local areas should develop a system wide strategic workforce plan (including a career framework) across health and care roles to ensure that they are able to recruit and retain the right skills and maintain the capacity and capability needed to deliver care to the local population.
Collaborative members identified the problems within local labour markets as a significant barrier to improving health and care outcomes. Years of financial restrictions and competition from other lower-paid employment opportunities have left the homecare provider market with a reduced ability to attract staff. Some 40% of iBCF monies from the plans we reviewed was spent on ‘stabilising the market’. About three quarters of this was used to increase care provider fees or to raise pay rates to meet national living wage requirements, rather than to add additional capacity or develop any innovative solutions to workforce constraints.
The local care market is a significant enabler of discharge and admission avoidance. However, many local authorities are currently struggling to provide sufficient capacity and ability to provide a service out of hours. A functioning intermediate care offer, which enables people to regain skills to live as independently as possible in their own homes, is therefore essential for improving hospital flow and reducing demand in the future.
In 2017/18, many local authorities invested in better remuneration for directly employed care providers. This is important but it isn’t enough – recruitment, career pathways, working environment, and training and development opportunities all need to be considered jointly with health partners. Technology also has a role to play in supporting the workforce to operate efficiently and effectively, and in enabling people to live independently.
There are some pockets of good practice around the country where local authorities have stabilised the homecare market, by focusing on outcomes and establishing mature relationships with providers (whether external or in-house) and health partners. Local authorities should build on this good practice and work with their health partners to develop a system-wide strategic workforce plan that enables them to develop a career framework across all health and care roles locally. This will help ensure that they are able to recruit and retain the right skills and capability to deliver care to their local population.
"Development of support and care in the community is vital to avoid admissions and enable people to return to the place they call home quicker. Supporting more people at home will require a significant shift of financial resources and workforce. The whole system needs to shoulder the responsibility to shift resources beyond sovereign responsibilities. It has been and remains a challenge to recruit to the health and social care sector in sufficient numbers to create the community-based support services we need to transform our services, leading to a continuation of meeting demand rather than reducing it. Better pay for the sector would help of course but we also need to work with providers and NHS partners to develop a new workforce offer for people wishing to work in the sector if we are to achieve our joint aims.”
Mike Alsop, Head of Integrated Commissioning, Warrington Borough Council
Recommendation 5: Change the narrative from coping with demand to maximising independence
Whitehall should cherish the concept of maximising independence, and should incentivise local government and healthcare providers to prioritise efforts related to improving long-term independence rather than hospital admissions or long-term care.
While the extra iBCF funding recognised that one part of the system (social care) could have a fundamental impact on the performance of another part (health), it was never going to be easy to deliver sustainable change in such a short timeframe. The cultural differences between the NHS and local councils’ Adult Social Care departments has been highlighted in their expectations of how the funding should be used and where it should have the greatest impact. The poor behaviours and actions of Government, regulators, lobbyists and interest groups in driving their own agendas over the last six months has inhibited local systems in delivering a sustainable future, with improved outcomes for people.
Central government needs to reframe health and social care. To create a sustainable health and social care system, they should move away from a narrative that focuses on trying to cope with demand at an organisational level and which may be driving people into long term care, towards one which emphasises independence and resilience, avoiding admission to hospital, and avoiding reliance on long-term care.
Achieving this relies in part on creating the right kind of environment at a national level to encourage local leaders to invest in admissions avoidance as well as creating the capacity and capability outside of hospitals and long-term care that can support efforts to maximise independence. That means putting in place the framework to incentivise medium term planning and encourage a co-ordinated approach in investing resources (time, money, people) in developing services, workforce planning and evidence. There are a few critical elements within the development of this framework:
- A resolution on the future of the Better Care Fund and more importantly system funding;
- Creating the right regulatory and political environment through appropriate and aligned system, organisational and personal incentives is vital in empowering local systems to take
responsibility for their actions; - Ensuring that appropriate financial risk sharing mechanisms are in place locally that incentivise
joint decision making but prevent risk transfer; - Ensuring performance reporting is managed locally based on local needs and is appropriate
for the level of investment
It also requires delivering this new narrative consistently across all relevant government departments and associated bodies.
"We need a new balance between the immediate and the important. This analysis shows that councils and their health partners made good progress in tackling the immediacy of delayed transfers of people from hospital. From here on there needs to be concentrated long term effort on reducing admissions to hospital by changing demand upon the health and care system. It is critical that central government develops the national framework that incentivises health and social care to achieve this aim locally.”
Peter Hay, Independent, Former Director of Adult and Children’s Services, Birmingham City Council
"Admissions avoidance is an important next step in managing performance, however I would like to see systems look beyond good performance as being only about admissions avoidance and quicker discharges. There is an emerging evidence base on developing healthy communities that focuses on improving people’s well-being and independence, which enables them to stay at home for longer. Investing in schemes that support these principles may not deliver an immediate improvement to system performance, but might be the only thing that sustains the health and social care system in the longer term. This is the challenge.”
Stephen Beet, Head of Service, Adult Care and Support, Bristol City Council
Concluding Comments
The additional funding for Adult Social Care has underlined central role that local authorities play in the health and care system alongside their NHS partners. By allocating the funding to local authorities, central government has recognised the pressures that local government is facing and its importance to supporting system flow in partnership with the NHS.
The funding has enabled health and social care to work more and better together, and there have already been some notable successes: a reduction in DTOC days being the most visible nationally. While iBCF wasn’t the only contributor to this reduction, it has certainly been a key enabler – not only in providing a funding stream to enable investment in social care markets and further changes, but also in raising the profile of adult social care in supporting this stepped change. Other successes include more constructive partnership conversations taking place at a local level. This must be encouraged, as many hospital admissions could be avoided through joint working in the community and at the front door.
Above all, taking an overview of what has been accomplished to date – and the funding that remains – there is a strong opportunity to increase focus on initiatives that address demand. This needs to be done jointly with health partners and national health and care bodies, through collaboration and a shared understanding of local issues and priorities. The groundwork for collaboration between the NHS and local authorities has been laid, and there is evidence of what can be achieved through joint working. The opportunity needs to be seized to embark on a journey towards sustainable health and social care services.
“The injection of new monies into social care has made a huge difference on our DTOC numbers and we have consistently been the best performing county across our system. This wouldn’t have been possible without our share of the £2 billion, which has enabled us to stabilise the home care and care home market at a time of rising costs, and put additional resource into hospitals. However, we now need to focus on the avoidance of hospital admission with the same relentless pursuit we applied to reducing delayed discharges.”
Joy Hollister, Strategic Director of Adult Care, Derbyshire County Council
Contributors
Many thanks to the following authorities who provided access to their data and shared the insights that made this report possible.

Related content
Read more related content from across the site, including in-depth reports, project case studies and articles.

