Consolidating the future of the NHS
Consolidating the future of the NHS
The NHS England planning guidance was published at the end of March, and the key word in the document is…
What the latest statistics from NHS England show is that practitioners seem to be getting much more efficient at getting people out of hospital beds. That hypothesis is substantiated when we look at the ratio of DTOC days to emergency admissions:
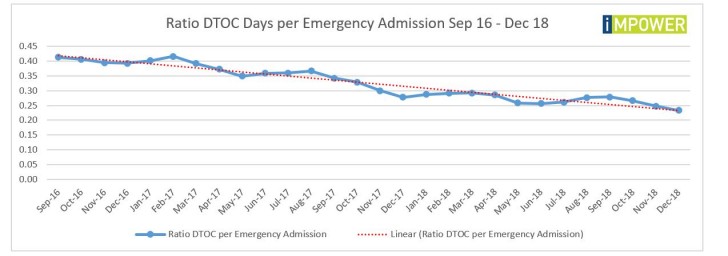
Despite that newfound efficiency, the deteriorating A&E performance and spiralling emergency admissions reveal that hospitals still can’t cope with demand at the front door. They are spiralling into what is almost affectionately called ‘winter pressures’, with hospitals on black alert, daily system calls focused on discharges and tensions running high.
Hitting the DTOC target (assuming that the target represents excellence in delays) is also a worry in that it would not help with those issues. Hitting the target would simply free up 87 beds across England….which would enable hospitals to accommodate an additional 6,371 emergency admissions each year (assuming an average length of stay of 5 days).
While there is always more that could be done, the problem of DTOC has basically been addressed. But the problem of demand most certainly has not; the front doors of our hospitals are quite simply overwhelmed. This is the wicked issue that needs to be addressed, and solving it would be a win-win-win: better outcomes for patients, reduced costs for the NHS and reduced costs for local authority departments of social care.
It is often said that ‘acuity has risen’. That might well be the case, but the same cohorts of people keep coming into hospital – and numerous studies (such as last year’s NAO report) have told us that at least 1 in 4 admissions could have been avoided.
The real solution to the annual winter crisis is not to keep obsessing about DTOC, and instead to reframe the problem away from ‘we can’t get people out of hospital beds’ and towards ‘people are not able to live independently in their own homes and are admitted to hospital too frequently’. But is anyone listening?
To see the ratio of DTOC days to emergency admissions for your local hospital, and other data, download the IMPOWER INDEX.